Uveitis
At Dhir Hospital , we are committed to providing our uveitis patients with advanced quality eye care at affordable prices.
- Home
- Service
- Uveitis

Overview
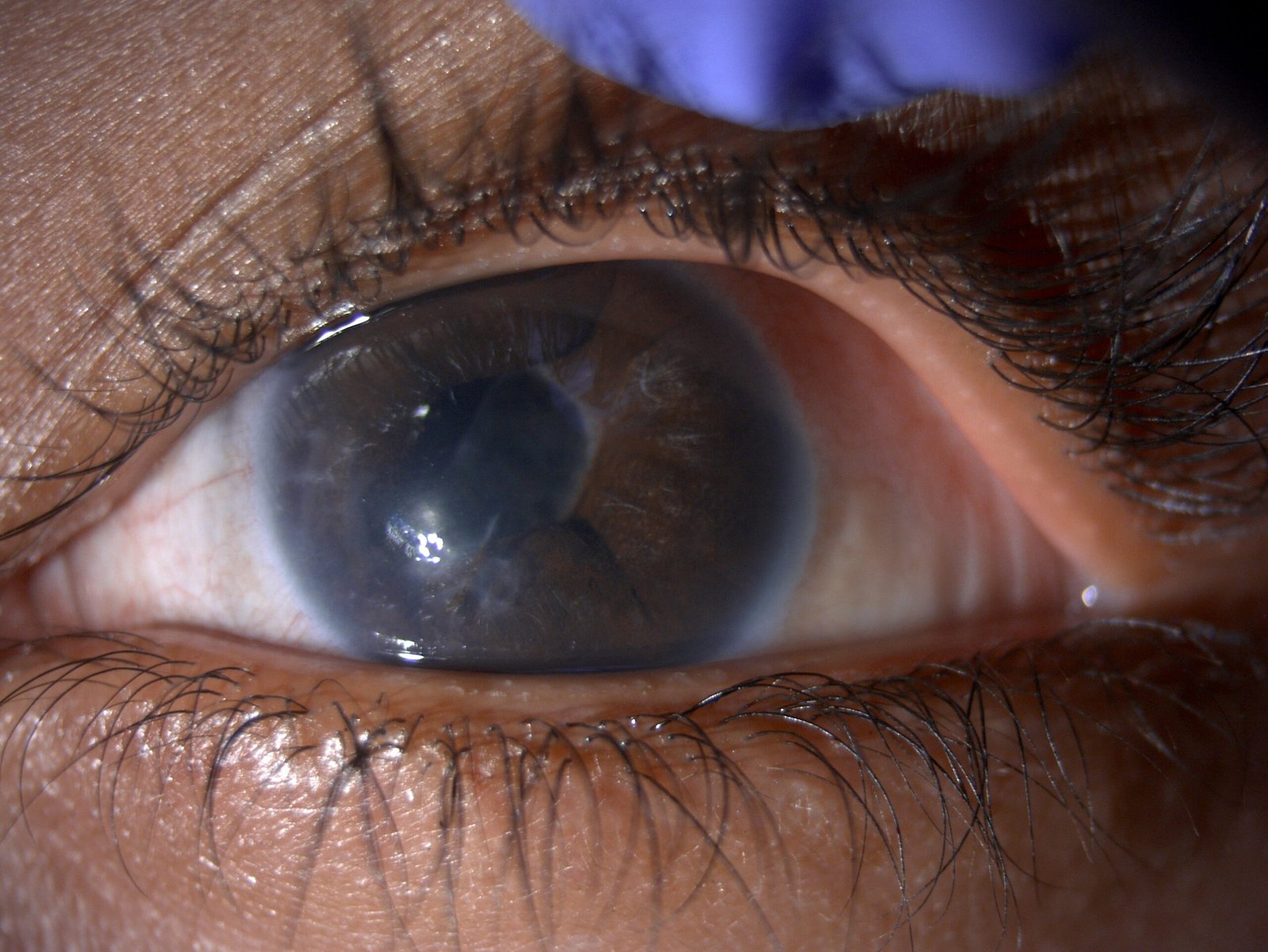
Uveitis is an eye inflammation affecting the middle layer of tissue in the eye wall (uvea). Warning signs of uveitis can suddenly show up, including redness, pain, and blurry vision in one or both eyes. It can happen to anyone, even kids.
Infections, injuries, or diseases that cause the immune system to react can lead to uveitis. Sometimes, though, the cause is unknown.
Uveitis is a serious condition that could result in permanent vision loss. Diagnosing and treating early is crucial to avoid problems and protect your vision.
Symptoms
Uveitis, an eye inflammation, can show these signs:
- Redness in the eye.
- Pain in the eye.
- Sensitivity to light.
- Blurry vision.
- Spots floating in your vision.
- Decreased vision.
- Symptoms may come suddenly or develop slowly, affecting one or both eyes. Sometimes, there might be no symptoms, and uveitis is found during a routine eye exam.
- The uvea, the middle eye tissue layer, includes the iris, ciliary body, and choroid.
- The iris is the colored part in front of the eye, the ciliary body is behind the iris, and the choroid is a blood vessel layer between the retina and sclera.
- The retina lines the inside of the back of the eye, and the gel-like vitreous fills the inside of the back.
Causes
In about half of cases, the cause of uveitis is unclear, possibly linked to an autoimmune disease specifically affecting the eyes.
Possible identified causes include:
- Autoimmune or inflammatory disorders affecting other body parts (e.g., sarcoidosis, lupus, Crohn’s disease).
- Ankylosing spondylitis is an inflammatory disease linked to spine and back issues.
- Infections like cat-scratch disease, herpes, syphilis, toxoplasmosis, or tuberculosis.
- Medication side effects.
- Eye injury or surgery.
- Very rarely, eye-related cancers like lymphoma.
Risk Factors
Uveitis, a condition causing eye inflammation, has several simple risk factors. You might be at risk if you have diseases that make your immune system overreact, like lupus or Crohn’s. Infections such as herpes or tuberculosis can also increase the chances of uveitis. Some medicines might have side effects leading to this eye issue. If you’ve had an eye injury or surgery, that can be a risk factor, too. Although rare, certain cancers like lymphoma can contribute. Sometimes, the cause of uveitis is unclear, making it important to know these factors for early detection and care.
Complications
If uveitis isn’t treated, it can lead to problems like:
- Swelling in the back of the eye (macular edema).
- Scarring on the retina.
- Pressure increases in the eye (glaucoma).
- Clouding of the eye’s lens (cataracts).
- Damage to the optic nerve.
- The retina pulls away from the back of the eye (retinal detachment).
- Permanent loss of vision.
Diagnosis
When you see an eye specialist, they’ll likely do a complete eye exam and ask about your health. Here’s what they might do:
- Check Your Vision: They’ll see how well you see, especially if you wear glasses.
- Eye Pressure Test: Using numbing eye drops, they’ll measure the pressure inside your eye.
- Slit-Lamp Exam: They’ll use a special microscope with a bright light to look at the front of your eye and check for tiny signs of inflammation.
- Eye Back Examination: They might dilate your pupils with drops and shine a light to look at the back of your eye.
Your doctor might also recommend:
- Color Photos: Pictures of the inside of your eye (retina).
- OCT Imaging: Mapping the layers of your eye to find any swelling.
- Angiography: Using a dye to take pictures of blood vessels in your eyes.
- Fluid Analysis: Taking a small sample of fluid from your eye.
- Blood Tests: Checking your blood for possible causes.
- Imaging Tests: Like CT or MRI scans to get more detailed pictures.
Treatment
When treating uveitis, the approach depends on the cause. If there’s an underlying condition, the focus is on treating that. However, the general goal is to reduce swelling in the eye, and sometimes, the treatment lasts months to years.
Medications:
- Anti-Inflammatory Drugs: Eye drops with medicine like corticosteroids are often prescribed to reduce swelling.
- Pupil Control: Some eye drops widen the pupil to ease spasms and relieve pain.
- Anti-Infection Drugs: Antibiotics or antiviral medications might be prescribed if uveitis is due to an infection.
Immune System and Cell-Affecting Drugs:
- Drugs affecting the immune system or destroying cells might be needed for severe cases.
Surgery or Other Procedures:
- Vitrectomy: Rarely used, this surgery removes some eye gel to diagnose or manage uveitis.
- Implants: A device releasing corticosteroid into the eye may be an option for complex cases.
These treatments may have side effects, like cataracts or glaucoma. Recovery speed depends on the type and severity of uveitis, with back-of-the-eye uveitis healing more slowly than front-of-the-eye uveitis. Regular follow-ups and tests are essential during treatment.
Preparing for the Appointment
Getting ready for your eye doctor appointment is essential, and here’s what you can do:
Before the Appointment:
- List Symptoms: Write down all your eye symptoms and anything else unusual happening in your body.
- Personal Information: Note any significant illnesses, traumas, or life changes.
- Medication List: Include all your medicines, vitamins, or supplements.
- Bring Someone: Having a friend or family member with you for support and remembering important details is helpful.
- Prepare Questions: Make a list of questions you want to ask your doctor.
Questions to Ask:
- What’s causing my eye problems?
- Are there other reasons for my symptoms?
- What tests do I need, and do I need to prepare for them?
- Is uveitis temporary or long-term?
- Will I lose my sight?
- What treatments do you recommend, and what are the side effects?
- Can I prevent this from happening again?
- How can I manage other health conditions along with uveitis?
- Can I take home any information about uveitis?
- Are there any websites you recommend?
Our Related Services
Glaucoma
At Dhir Hospital, we provides the best Glaucoma Treatment in Bhiwani, Haryana with experienced Glaucoma Surgeons.

Lasik & Refractive Surgery
Lasik eye surgery is considered one of the best methods for the correction of refractive errors. Contact Dhir Hospital to get treated by the best eye specialists for Lasik and refractive surgery in Bhiwani, Haryana.

Paediatric Ophthalmology
Dhir Hospital has the best pediatric ophthalmologists in Bhiwani, Haryana to treat ophthalmology disorders in children. Book an appointment

Ophthalmic Plastic and Facial Aesthetic Surgery
Searching for the best oculoplastic surgeon In Bhiwani, Haryana? Contact Dhir Hospital to get treated by the best eye specialists for eyelid surgery in Bhiwani, Haryana..
FAQ
Frequently Ask Questions.
Uveitis is an inflammation of the uvea, which includes the iris, ciliary body, and choroid. It can affect one or both eyes and can be categorized as anterior uveitis (inflammation in the front of the eye), intermediate uveitis (inflammation in the middle part of the eye), posterior uveitis (inflammation in the back of the eye), or panuveitis (inflammation affecting all parts of the eye).
Uveitis can have various causes, including infections (such as viral, bacterial, or fungal), autoimmune disorders, trauma or injury to the eye, certain medications, or underlying systemic diseases. In some cases, the cause may remain unknown.
Diagnosis of uveitis involves a comprehensive eye examination, including visual acuity testing, slit-lamp examination, and sometimes additional tests like fluorescein angiography or optical coherence tomography (OCT) to assess the severity and extent of inflammation.



