Retina & ROP
At Dhir Hospital, we provides the best Retina Treatment in Bhiwani, Haryana with experienced Retina Surgeons.
- Home
- Service
- Retina & ROP
Overview
Retinal diseases can impact the thin layer at the back of your eye, known as the retina, which plays a crucial role in vision. This area consists of light-sensitive cells like rods, cones, and nerve cells that process visual information and transmit it to the brain through the optic nerve. Visible symptoms are common with retinal diseases and can affect various parts of the retina.
If you experience retinal issues, seeking care from a retinal specialist is essential. These specialists can provide treatment options depending on the disease, with goals such as slowing or stopping the progression and preserving, improving, or restoring vision. It’s crucial to address retinal diseases promptly, as untreated conditions can lead to severe vision loss or even blindness.
Types
Common retinal diseases and conditions include:
- Retinal Tear: This happens when the gel-like substance (vitreous) in your eye pulls on the thin tissue at the back (retina), causing a break and symptoms like floaters and flashing lights.
- Retinal Detachment: Fluid under the retina leads to detachment, often occurring through a retinal tear.
- Diabetic Retinopathy: In diabetes, blood vessels in the eye can deteriorate, leaking fluid into the retina, causing swelling and vision issues.
- Epiretinal Membrane: A scar or membrane on the retina can distort vision, making objects appear blurred or crooked.
- Macular Hole: A minor central retina defect leading to blurred vision, often caused by abnormal traction or eye injury.
- Macular Degeneration: Deterioration of the central retina resulting in blurred vision or a blind spot. There are wet and dry forms.
- Retinitis Pigmentosa: An inherited disease causing a slow night and side vision loss.
Symptoms
Common signs and symptoms of retinal diseases include:
- Seeing floating specks or cobwebs
- Blurred or distorted vision
- Defects in the side vision
- Lost vision
Risk factors
Risk factors for retinal diseases might include:
- Aging
- Family history of retinal disorders
- Diabetes
- High blood pressure
- Smoking
- Eye injuries or trauma
- Prolonged exposure to sunlight
- Certain genetic factors
Diagnosis
To diagnose retina problems or retinal diseases, a retinal specialist may conduct various tests during a comprehensive eye exam. These tests include:
- Amsler Grid Test: Your retinal specialist may use an Amsler grid to assess the clarity of your central vision, identifying any distortions or abnormalities that could indicate retinal issues.
- Optical Coherence Tomography (OCT): This imaging technique provides detailed retina pictures and diagnoses conditions such as macular degeneration, macular holes, and macular swelling.
- Fundus Auto fluorescence (FAF): FAF helps evaluate the progression of retinal diseases by highlighting specific pigments associated with retinal damage.
- Fluorescein Angiography: This test uses a dye to highlight blood vessels in the retina, assisting in identifying various vascular issues and abnormalities.
- Indocyanine Green Angiography: Employing a dye that reacts to infrared light, this test reveals blood vessels in the choroid, providing insights into deeper retinal structures.
- Ultrasound: High-frequency sound waves are used to view the retina and assess characteristics contributing to diagnosing and treating eye tumors.
- CT and MRI: In rare instances, these imaging methods may be used to evaluate eye injuries or tumors, providing additional information for diagnosis and treatment planning.
A retinal specialist can identify and diagnose various retinal problems through these tests, allowing for appropriate management and treatment. Regular visits to a retinal specialist are crucial for individuals experiencing symptoms or at risk of retinal diseases.
Treatment
Treating retinal diseases primarily aims to halt or slow disease progression and maintain, enhance, or restore vision. Early detection is crucial since the damage that has occurred may be irreversible. Treatment options can be complex and, at times, urgent. Here are various approaches:
- Laser Surgery: Utilizing a laser can repair a retinal tear or hole by creating scarring that binds the retina to underlying tissue. Immediate laser treatment can reduce the risk of retinal detachment.
- Shrinking Abnormal Blood Vessels: Scatter laser photocoagulation may be used to shrink abnormal blood vessels threatening to bleed into the eye, particularly in cases of diabetic retinopathy.
- Freezing (Cryopexy): A freezing probe is applied to the eye’s external wall to treat a retinal tear. Intense cold freezes the retina, leading to scarring that secures it to the eye wall.
- Injecting Air or Gas: Pneumatic retinopexy involves injecting air or gas into the eye to repair certain types of retinal detachment. This may be combined with cryopexy or laser photocoagulation.
- Scleral Buckling: This surgery indents the eye’s surface by sewing a small piece of silicone material to the outer eye surface. It helps relieve force caused by vitreous tugging on the retina, facilitating reattachment.
- Vitrectomy involves removing the gel-like fluid inside the eye and injecting air, gas, or liquid into the space. It’s used for conditions such as retinal tears, diabetic retinopathy, macular holes, and retinal detachment.
- Injecting Medicine into the Eye: Medication may be injected into the vitreous to treat conditions like wet macular degeneration, diabetic retinopathy, or broken blood vessels within the eye.
- Retinal Prosthesis Implant: A tiny electrode chip is implanted in the retina for severe vision loss due to inherited retinal diseases. It receives input from a camera on eyeglasses, relaying visual information that the damaged retina can no longer process.
Preparing for your appointment
To check for retina problems or retinal diseases, you’ll need a dilated eye exam from a specialized doctor like a retinal specialist, an optometrist, or an ophthalmologist. Before your appointment, ask about any preparations required. Make a list of symptoms, medications, and supplements. Having someone accompany you is advisable as your vision may be affected post-dilation.
Questions to ask the doctor about retina problems include the severity of the condition, safety for activities like driving, the potential for further vision loss, available treatments, and the role of supplements. Discuss monitoring methods, signs to report, low-vision aids, lifestyle changes, and preventive measures. During the appointment, expect questions about when you noticed the issue, its impact on one or both eyes, difficulties with near or distant vision, smoking history, other health conditions, family history of retinal disease, and any eye injuries.
Our Related Services
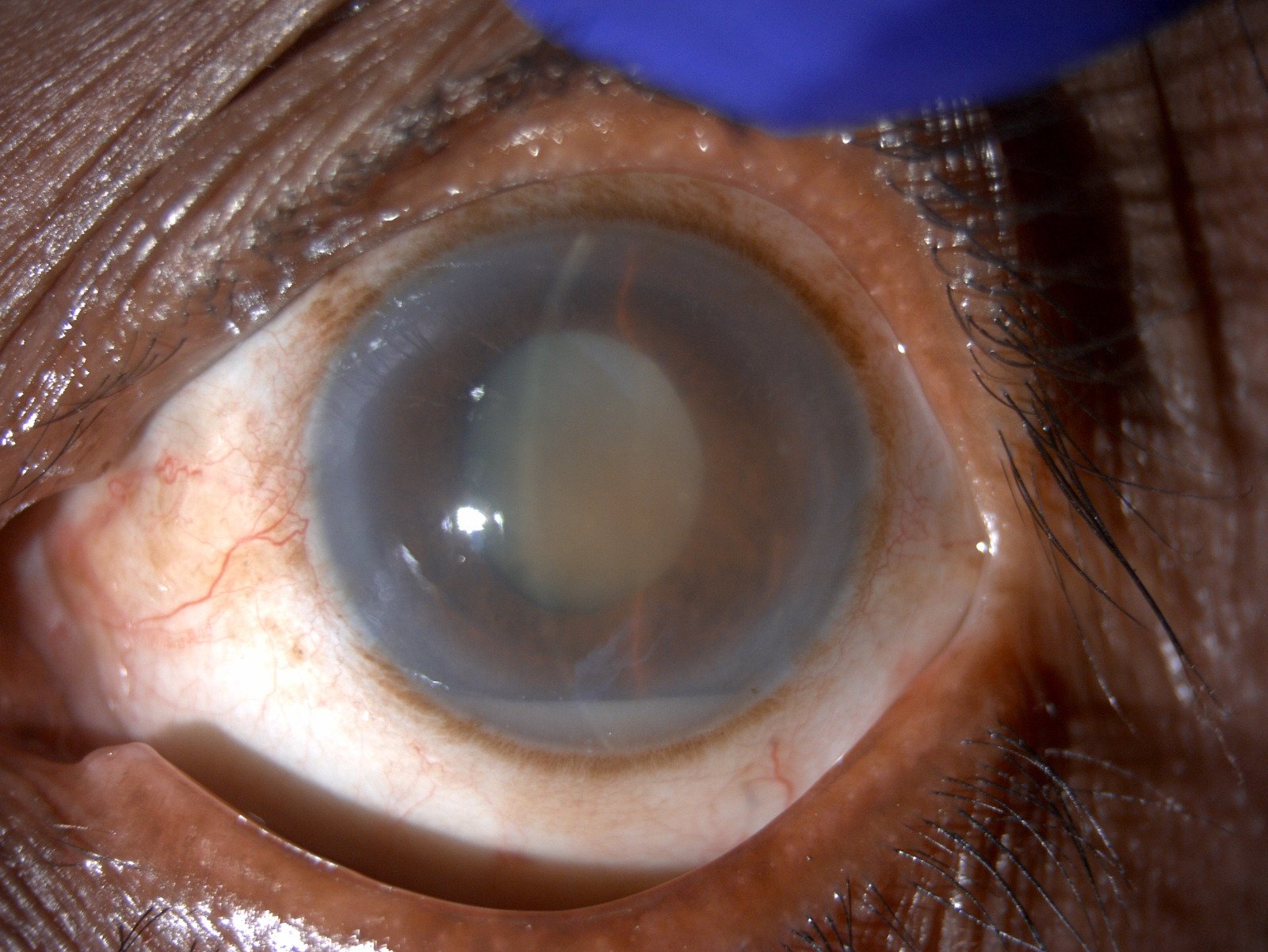
Cataract & Anterior Segment
Dhir Hospital has the best Cataract & Anterior Segment in Bhiwani, Haryana with decades of experience. We offer All types of lenses & cataract Rx. Book your appointment
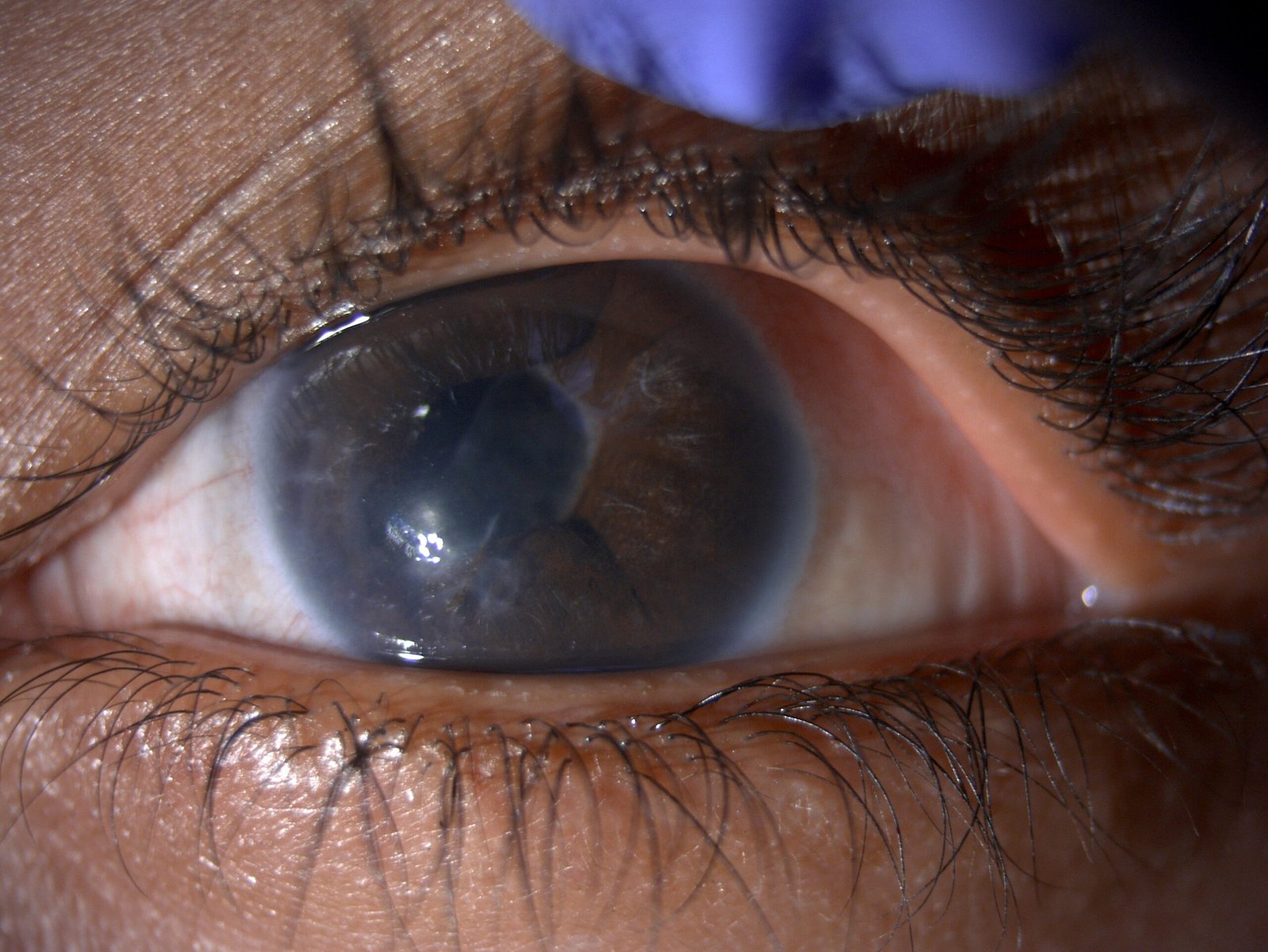
Glaucoma
At Dhir Hospital, we provides the best Glaucoma Treatment in Bhiwani, Haryana with experienced Glaucoma Surgeons.

UVEITIS
At Dhir Hospital , we are committed to providing our uveitis patients with advanced quality eye care at affordable prices.

Lasik & Refractive Surgery
Lasik eye surgery is considered one of the best methods for the correction of refractive errors. Contact Dhir Hospital to get treated by the best eye specialists for Lasik and refractive surgery in Bhiwani, Haryana.
FAQ
Frequently Ask Questions.
Why should I worry about the eyes of a premature baby?
It is important to be concerned about the eyes of a premature baby because their delicate eyes are more vulnerable to complications and developmental issues. Premature babies have underdeveloped blood vessels in their retinas, which can lead to a condition called retinopathy of prematurity (ROP).
ROP can cause abnormal blood vessel growth and potentially lead to vision loss or even blindness if left untreated. Therefore, close monitoring and timely intervention are crucial to ensure the healthy development of a premature baby's eyesight.
How can we detect ROP?
ROP (retinopathy of prematurity) can be detected through a comprehensive eye examination by an ophthalmologist. This involves pupil dilation, retinal examination, and possibly imaging tests. Early detection is important for timely intervention and treatment. Regular follow-up visits are crucial for monitoring the condition.
Do all babies need a retinal examination for ROP?
Not all babies require a retinal examination for retinopathy of prematurity (ROP). The need for an examination depends on certain risk factors, including the baby's gestational age, birth weight, and overall health. Generally, premature babies born before 30 weeks of gestation or weighing less than 1500 grams are at higher risk for developing ROP and are more likely to undergo retinal examinations. However, it is ultimately up to the healthcare provider to determine if an examination is necessary based on the individual baby's circumstances.
Is it too late for my baby's eyes?
It's important to follow the "Day-30" strategy for premature babies' eyes. This means that the first retinal examination should ideally be done before the baby reaches 30 days of life. However, it is even better to have the examination done earlier, around 2-3 weeks after birth, especially for babies with very low birth weight (less than 1200 grams). This strategy is a reminder that timely screening within the first 30 days can play a crucial role in preserving your baby's vision. So, remember, "Thirty Days to Vision - Tees Din Roshni ke!"
What is the treatment for ROP?
The treatment for Retinopathy of Prematurity (ROP) can vary depending on the severity of the condition. Some common treatment options include:
- Laser Treatment: Laser therapy is the most common approach for treating ROP. In this procedure, a laser is used to target and destroy the abnormal blood vessels in the retina. By doing so, it helps prevent further growth and reduces the risk of retinal detachment.
- Injections: In certain cases, injections of medication, such as anti-VEGF (vascular endothelial growth factor) drugs, may be used to stop the growth of abnormal blood vessels and promote healthy retinal development.
- Cryotherapy: Cryotherapy involves using freezing temperatures to destroy abnormal blood vessels. This treatment is typically used for more advanced stages of ROP.
- Surgery: In some severe cases of ROP, surgical intervention may be necessary. Surgical options can include vitrectomy, which involves removing the gel-like substance inside the eye, or scleral buckling, which involves placing a silicone band around the eye to support the retina.
The choice of treatment will depend on various factors, including the stage and location of ROP, as well as the individual baby's condition. It is essential to consult with a qualified ophthalmologist who specializes in treating ROP to determine the most suitable treatment approach for your baby.
How often should the retina be examined?
ROP can worsen in just 7-14 days, so it's important to closely monitor it until the retina fully matures. Multiple examinations may be necessary before your baby is out of danger. Don't skip ROP follow-up appointments as each visit is crucial for their well-being.
When should we treat ROP?
Treating ROP promptly, ideally within 72 hours or sooner, is incredibly important when it reaches a critical stage called High risk pre-Threshold ROP or aggressive ROP (AROP). If treatment is delayed beyond this point, there is a substantial risk of vision loss. Time is truly crucial in safeguarding the best possible outcome for your baby's vision health.
After treatment
When treated promptly, the child can expect to have reasonably good vision. It's important for all premature babies to undergo regular eye exams until they start school. There may be a need for glasses or treatment for conditions like lazy eyes, cross-eyes, cataracts, glaucoma, and retinal detachment.
A laser is like a powerful beam of light that can be used to treat specific areas of the retina without affecting the surrounding tissues. It creates a tiny spot of energy to either destroy lesions or join tissues together. Laser surgery is typically painless, although some people may feel temporary discomfort. It's usually done in an operating room while the patient is awake and comfortable. In rare cases, anesthesia may be given to those who can't handle the discomfort or to children who need to stay still during the treatment. The whole procedure usually takes around 10 to 30 minutes.
Who requires laser treatment?
Laser treatment may be required for individuals with certain eye conditions or diseases. These can include conditions such as diabetic retinopathy, retinal tears or detachments, macular degeneration, and certain types of glaucoma. Laser treatment is often used to prevent further damage or to treat specific areas of concern in these conditions. The decision to undergo laser treatment is typically made by an eye care professional based on the individual's specific needs and circumstances.
Diabetic Retinopathy
The blood vessels in the retina are like pipes that bring blood into and out of the back of the eye. However, in diabetes, these vessels can leak, causing the retina to swell and function improperly. This can lead to vision problems, especially if the central area of the retina is affected, which is known as diabetic macular edema.
Laser treatment can help by sealing these leaks, preventing further vision loss. In some cases, diabetes can cause new blood vessels to grow in the retina, known as proliferative diabetic retinopathy. However, these new vessels are fragile and can bleed inside the eye, causing decreased vision. Laser treatment can often stop the progression of these vessels and prevent severe vision loss.
Retinal Vein Occlusion
Retinal vein occlusion, which is more common in patients with diabetes or high blood pressure, can lead to swelling of the retina due to fluid and blood buildup. This can cause blurry vision in both the center and periphery. In some cases, the condition may also result in the growth of new blood vessels, causing pain and high pressure inside the eye known as neovascular glaucoma. Fortunately, laser treatment can help alleviate the swelling and make the new blood vessels disappear.
Age Related Macular Degeneration (AMD)
With age, some individuals may experience changes in the macula, the part of the retina responsible for our central reading vision. The majority of people develop the dry type of age-related macular degeneration (AMD), which leads to gradual vision loss. However, the more severe wet type causes the macula to swell with fluid and blood. Common symptoms of wet AMD include painless, blurred, and distorted vision. In urgent cases, laser surgery can be performed to prevent or delay further vision loss. For those with off-center wet AMD, thermal laser treatment can be beneficial, while individuals with central vision problems may require an injection of Visudyne prior to undergoing photodynamic therapy.
Retinal Breaks and Retinal Detachment
The retina, which lines the back of the eye like a wallpaper, can develop tears or rips as we age or due to certain eye conditions or injuries. When a retinal tear occurs, patients may experience cobweb-like floaters or flashes of light. If the liquid in the central part of the eye (vitreous) leaks beneath the tear, it can cause the retina to detach from the eye wall. This condition, known as retinal detachment, can lead to blindness if not treated promptly. Fortunately, laser surgery performed around the retinal tears, before fluid accumulates, can help surgeons secure the retina to the underlying eye wall. This procedure can prevent or reduce the risk of retinal detachment.
Central Serous Chorioretinopathy (CSCR)
Central Serous Chorioretinopathy is a condition where fluid-filled blisters form beneath the macula. This can lead to reduced and distorted vision, abnormal color perception, a central blind spot, and temporary far-sightedness. While most cases resolve without intervention, laser photocoagulation may be needed for persistent blisters or for patients seeking early visual improvement.
Ocular Tumors
In some cases, patients may experience swelling and dysfunction of the retina due to non-cancerous vascular tumours that leak. Laser surgery can be used to target and destroy these tumors, helping to alleviate the swelling and restore proper retinal function.
What is laser treatment of the retina?
Laser treatment of the retina is a medical procedure that uses a focused beam of light energy to treat various conditions affecting the retina, the light-sensitive tissue at the back of the eye.
What conditions can be treated with laser treatment?
Laser treatment of the retina is commonly used to address conditions such as diabetic retinopathy, retinal tears or detachments, macular degeneration, and certain types of glaucoma.
How does laser treatment work?
During laser treatment, the focused beam of light energy is precisely directed onto the retina. It can be used to seal leaking blood vessels, reduce swelling, destroy abnormal blood vessels, or create tiny burns to repair retinal tears or detachments.
Is laser treatment painful?
Laser treatment is usually painless, with most patients experiencing only minimal discomfort. In some cases, there may be a sensation of warmth or a brief stinging feeling during the procedure. Anaesthesia is typically not required.
How long does a laser treatment procedure last?
The duration of a laser treatment procedure can vary depending on the specific condition being treated and the extent of the area involved. Generally, the procedure lasts between 10 to 30 minutes.
Are there any side effects or risks associated with laser treatment?
While laser treatment is generally considered safe, there can be some potential side effects. These may include temporary blurring or distortion of vision, sensitivity to light, or mild discomfort. Serious complications are rare but can include infection or damage to surrounding tissues.
What is the recovery process after laser treatment?
Recovery after laser treatment is typically quick and straightforward. Patients can usually resume their normal activities immediately after the procedure, although some may experience mild redness or irritation in the treated area for a short period.
What is diabetic disease of the retina?
Diabetic disease of the retina, also known as diabetic retinopathy, is a complication of diabetes that affects the blood vessels in the retina. Over time, high blood sugar levels can damage these blood vessels, leading to vision problems and potential blindness.
What are the symptoms of diabetic disease of the retina?
In the early stages, there may be no noticeable symptoms. As the disease progresses, symptoms may include blurred or fluctuating vision, dark spots or floaters, difficulty seeing at night, and even complete vision loss if left untreated.
Who is at risk of developing diabetic disease of the retina?
Anyone with diabetes, whether it is type 1 or type 2, is at risk of developing diabetic retinopathy. The risk increases with the duration of diabetes, poor blood sugar control, high blood pressure, and high cholesterol levels.
How is diabetic disease of the retina diagnosed?
An eye examination by an ophthalmologist or optometrist is necessary to diagnose diabetic retinopathy. The doctor will perform various tests, including a dilated eye exam, to check for any abnormalities in the retina's blood vessels.
What are the treatment options for diabetic disease of the retina?
Treatment options for diabetic retinopathy depend on the severity of the condition. In the early stages, managing diabetes through lifestyle changes, such as maintaining a healthy diet and regular exercise, along with strict blood sugar control, may help slow down the progression. In more advanced cases, treatments like laser therapy, injections, or surgery may be recommended to prevent further vision loss and preserve eye health.
Are there any complications associated with diabetic disease of the retina?
If left untreated, diabetic retinopathy can lead to several complications, including macular edema (swelling of the central part of the retina), macular ischemia (decreased blood flow to the macula), retinal detachment (separation of the retina from its underlying tissue), and even permanent vision loss or blindness.
How often should someone with diabetes get their eyes checked for diabetic retinopathy?
It is recommended that individuals with diabetes undergo a comprehensive dilated eye exam at least once a year. However, if you already have signs of diabetic retinopathy, your eye doctor may recommend more frequent exams, depending on the severity of the condition.










